| |
|
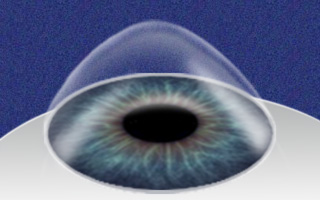
Keratoconus
Keratoconus is an eye disease that
concerns the cornea. The cornea is a thin, clear tissue covering
the surface of the front of the eye.
It is a very
important contributor to our vision, accounting for 2/3 of the
eye's optical power. A normal, healthy cornea holds its round
shape and helps us see.
But sometimes the cornea becomes
structurally weakened and loses its shape. Instead of a dome, it
becomes cone-shaped, prohibiting clear vision. This is known as
keratoconus. |
 |
Causes of keratoconus
The cause of keratoconus
is unknown. Some research shows that keratoconus may run in families and
may affect those with allergies more often. Other research suggests too
much eye rubbing can cause keratoconus. Although it is not proven that
eye rubbing can exacerbate keratoconus, it is probably a good idea to
keep from rubbing the front of your eye too much anyway, as it is a
delicate part of the body.
Most of the time, there is no eye injury
or disease that provokes keratoconus. If you develop keratoconus, you
were probably bound to develop it from birth. Keratoconus is most
prevalent in those who are near-sighted.
There are no
preventative measures for keratoconus, but if you develop it, there are
many treatment options available.
Onset
and Treatment
Keratoconus usually develops early, in
the teenage years and twenties, but it can begin even earlier,
during childhood.
It will most likely present in a
patient before age 30. Keratoconus can progress for 10-20 years
and then slow down considerably as the patient ages.
The
first symptoms of keratoconus are blurred vision and increased
sensitivity to light. At first, you may be able to wear soft
contact lenses or eyeglasses to correct the mild
near-sightedness and/or astigmatism caused by keratoconus.
Eventually keratoconus may progress so far that glasses cannot
correct your vision. |
 |
Advanced Treatment
Usually keratoconus can be
corrected over a lifetime using rigid gas-permeable contact lens and
regular check-ups. In advanced cases, the cornea wears down at the very
point of the cone shape. If this happens, you may need to undergo a
corneal transplant. Recovery from this surgery can take a long time, but
the risk of the body rejecting a transplanted cornea is very low. Most
often, patients will still need to wear contact lenses after the
surgery.
There are a few different options to prevent the need for a
corneal transplant:
• Intrastromal corneal ring segments: a
surgical procedure where small implants are inserted into the eye to
correct vision.
• Mini asymmetric radial keratotomy: a
controlled scarring of the cornea by administering a careful pattern of
incisions. Scar tissue develops around the incision points and reshapes
the cornea.
• Corneal cross-linking: a method where custom
riboflavin eye drops are activated by ultra-violet light over a
30-minute session, meant to increase collagen cross-linking in the
cornea and thereby strengthen it.
Diagnosis
To test for keratoconus, your eye doctor will check for distorted
vision, blurred vision of objects (both near and far), sudden changes in
one eye's vision or double vision when using only one eye and halos
around bright lights.
Keratoconus can be diagnosed by
examination. A slit-lamp examination may be performed. A
slit-lamp is a kind of low-power microscope that shines a bright
beam of light into the eye. This examination can be used to
detect many eye diseases and problems, including corneal
injuries, cataracts and macular degeneration (a disease of the
macula, the part of the eye that allows you to see fine
details). |
 |
Another type of examination called corneal topography can be performed
using computerized instruments to create a map of the cornea. This is an
advanced technology and offers the most complete view of your cornea.
If you are considering corrective laser eye surgery,
it is imperative you do not even have borderline keratoconus. Corneal
topography will be performed on any patient seeking LASIK treatment to
make sure they do not have keratoconus before scheduling surgery.
Prevention
Although there are no specific ways
to prevent keratoconus, some basic lifestyle choices can help keep your eyes healthy.
• Regular eye examinations are a
must. It is during these exams that your health care provider has a
chance to detect any conditions like keratoconus before they become a
bigger problem. Once a year check-ups are instrumental in maintaining
health vision over your lifetime.
• Wearing sunglasses to protect your eyes is
an easy way to guard your vision against UV damage.
•
A healthy lifestyle keeps your blood pressure, cholesterol and blood
sugar in balance. Suggestions include no smoking, limited alcohol
consumption and lots of leafy, green vegetables high in antioxidants.
When to see a eye care professional:
If your
child or teenager has vision problems that cannot be corrected to 20/20
with glasses, they should be evaluated by a eye care professional with
experience in diagnosing and treating keratoconus.
Always see
your eye care professional immediately if you
have any sudden changes in vision. This includes darkening around the
edges of your vision, dark spots in front of your eyes, halos around
bright lights, a loss of vision in one part of your field of sight or
any other noticeable change.
|
| |
|