|
Retinoschisis
Age related retinoschisis is a degenerative
process occurring in the retina, beginning at
the inner front part of the eye nearest the
iris. This area slowly enlarges becoming filled
with a viscous (thick) substance, filling up
like a balloon.
This process advances until the involved retina
is completely separated into two degenerated
layers, severing the neuronal elements and
resulting in complete and permanent loss of all
visual function in the involved area (i.e. a
blind spot). |
|
 |
|
Degenerative retinoschisis
has a prevalence of 3.7% among patients over age
10, and of 7% among those over 40 years of age.
Two forms have been described. One form
designated flat (or typical) was thought to be a
milder form, versus the other form designated
bullous (or reticular, balloon-like), thought to
be more severe. It is, however, impossible to
differentiate these types of lesions into these
categories reliably.
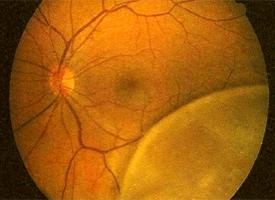
Clinically, degenerative retinoschisis usually
presents as a peripheral, smoothly elevated
lesion, with a uniformly convex posterior
border. It appears as a “water blister” on the
retina. The surface of the lesion may show
whitened blood vessels, or areas of small
whitish flecks called Gunn’s dots. Retinal
breaks, as seen in the above photograph, may
eventually appear in the outer layer in around
15% of involved patients. Breaks in the outer
layer may be of any size, but frequently are
huge, and are usually seen to have a prominent
whitish rolled border.
It has been long known that these retinal breaks
occur in as many as 11% of affected eyes and may
be associated with retinal detachment. It has
been reported that a schisis-detachment occurs
in around 8% of patients with retinoschisis, as
opposed to the frequency of retinal detachment
in the natural population of 0.05% (or 1 in
2000) patients.
In almost all cases of degenerative
retinoschisis (at least 99%), the disease
produces no symptoms. Therefore, most existing
cases are never discovered. Its presence usually
comes to light only when the patient consults
their optometrist because of other symptoms,
such as those related to a posterior vitreous
detachment (PVD). Actual progression of the
retinoschisis to involve the macula is
exceedingly rare.
Patients with retinoschisis should be followed
every 6 to 12 months if no symptoms are
reported. However, they should be examined
promptly if any change is noted. Patients with
retinoschisis should be educated about the signs
and symptoms of retinal detachment. Patients
need to understand that delaying the reporting
of the sudden appearance of flashes of light,
floaters, sparkles of light, or shadows, can
seriously increase the risk of permanent vision
decrease or loss.
Treatment of retinoschisis should only be
considered in cases of symptomatic, progressive
retinal detachment. It has never been shown that
prophylactic treatment statistically preserves
vision or prevents complications in cases of
degenerative retinoschisis. |